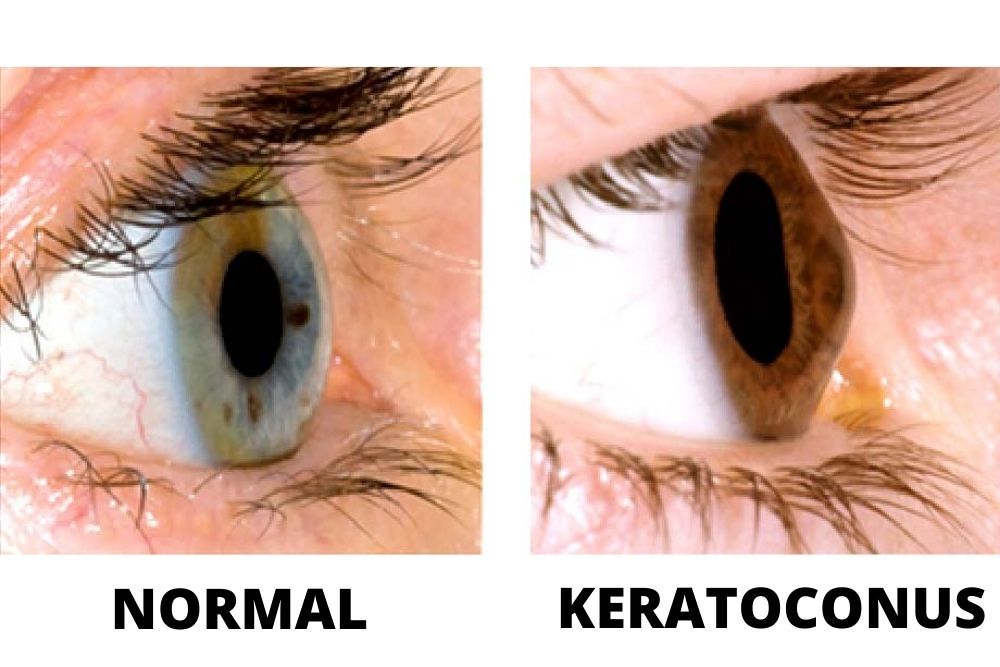
Keratoconus is when the cornea bulges outward forming a cone shape in your eye. The cornea is the clear, dome-shaped surface of your eye that causes blurred vision and light sensitivity when deformed.
Keratoconus usually occurs in both eyes but is often more severe on one eye than the other. It usually affects people progressively between the ages of 10 to 25.
Glasses and special contact lenses are usually used to treat the early stages of keratoconus. However, keratoconus that has progressed severely may require a corneal transplant. The new treatment, corneal collagen cross-linking, claims slow the progression of keratoconus which could prevent future surgeries.
Symptoms
As keratoconus progresses, signs and symptoms may vary but would normally include:
- Distorted or blurry vision
- Light and glare sensitivity
- Poor night vision
- Double vision
- Sudden clouding or worsening of vision
- Fast-progressing eyeglass prescription
Causes
Collagen, the tiny protein fibers, hold the cornea in place and prevents it from bulging away from the eyes. When the collagen weakens, they can no longer hold the cornea in place making its shape similar to a cone.
The cornea cells normally produce damaging by-products over time, like exhaust from a vehicle. Generally, the antioxidants that the body produces get rid of harmful by-products and protect the collagen fibers in the eyes. If the body cannot produce enough antioxidants, the collagen weakens and the cornea starts to bulge out which could progress into severe keratoconus.
There is no direct cause as to why keratoconus occurs, although genetic and environmental factors are believed to be involved. Studies show that about 1 in 10 people with keratoconus have at least one parent with the condition. This is why experts advise parents with the condition to have their children’s eyes checked from age 10 onwards.
Risk Factors
Other medical problems, such as allergies and chronic eye rubbing are said to speed up the progression of keratoconus. Here are other factors that can increase your odds of developing keratoconus:
- Having a family history of keratoconus
- Having specific conditions like retinitis pigmentosa, Ehlers-Danlos syndrome, Down syndrome, asthma, and hay fever
The changes in the shape of the cornea can occur rapidly over a short period of time which may result in blurred vision, light sensitivity, glare and halos at night, and poor night vision.
Complications
In some cases, the cornea may swell suddenly and cause abrupt diminished vision and scarring of the cornea. This is caused by a phenomenon in which the lining inside your cornea breaks down and allows fluid to penetrate the cornea (hydrops). The swelling normally recedes by itself, but a scar may form irreversibly especially where the cone is most prominent. This could worsen your vision and may require cornea transplant surgery.

Diagnosis
Keratoconus can change vision in two ways:
- Cornea changes from a dome-shaped to a cone shape. This is a type of keratoconus where the smooth surface becomes distorted. This is referred to as irregular astigmatism.
- Cornea expands. If the cornea expands instead of protruding, vision becomes nearsighted.
An eye doctor will roll out a few eye exams, check for possible keratoconus symptoms, and measure the shape of your cornea to properly diagnose keratoconus.
The most common technique that eye doctors use to measure the shape of the cornea is corneal topography. This method snaps an image of the cornea and analyzes it within seconds. Children with parents who have keratoconus are advised to undergo a cornea topography at least once a year from age 10. This is to properly monitor any signs of keratoconus and prevent it from progressing rapidly.

Treatment
Treatment usually begins with prescription eyeglasses. If eyeglasses can no longer provide normal vision, then rigid gas permeable or scleral contact lenses are prescribed for better vision.
Cornea collagen crosslinking is a surgical option to effectively prevent the worsening of keratoconus. Intacs are implants that are positioned under the surface of the cornea to lessen the cone shape and enhance vision.
A technoscientific laser procedure, PTK, can smoothen out a raised scar on the cornea and improve contact lens comfort. However, if the keratoconus has progressed to a greater degree, a cornea transplant can be performed. This means removing the middle part of the cornea and replacing it with a donor cornea which is stitched into place. This is customarily only done as a last hope.
Beware of laser vision correction surgery. Anyone with even a small degree of keratoconus should not have LASIK surgery as this could further weaken the cornea and make vision worse.
When to see a doctor
Even if your child’s corneal topography appears to be normal, it is still necessary to have this test conducted yearly. subtle changes may appear over time which may indicate the onset of the disease. With yearly eye exams, your doctor can compare results to identify any changes as early as possible.
See your eye doctor immediately if you experience any sudden worsening of vision and if you notice any changes and irregularities in the curvature of your eye.



